Population Health Management
By Matthew Bavolack, National Healthcare Services Leader

Population Health Management (PHM) are we ready? You shouldn’t be asking this question at this point.
What is PHM? PHM is an ongoing shift in the delivery of care that has been trending for almost a decade. In basic terms, it’s a shift from VOLUME to VALUE. We all saw this with the introduction of the ACO marketplace, the continued increase in Medicare Advantage (MA) plan usage, and the Bundled Payment & Care Initiatives (BPCI), which, interestingly enough, have grown over the last five years by as much as 100% in some regions.
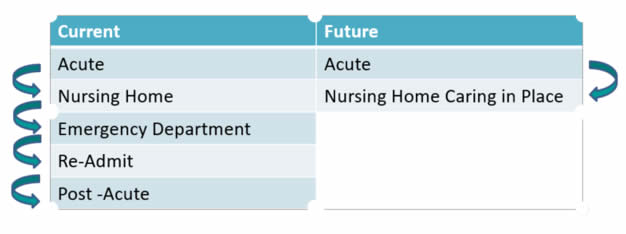
The goal of PHM is to continue the shift in the delivery of care to provide care in place and to reduce overall hospital readmissions. Let’s look at the before and after model.
How do we “care in place” and what does it mean?
Presently, the care delivery system follows a hierarchical payment model. CMS contracts with a Medicare access agency, the Medicare access agency charges a fee to CMS for administrative services and then pays the provider, and the provider uses funds to care for residents. Caring in place affords the provider the ability to provide needed skilled services to an individual without hospital readmission, hence reducing the cost of care and aligning finance and quality. This is accomplished through the use of Special Needs Providers (SNPs):
- I-SNP (Institutional)
- C-SNP (Chronic)
- D-SNP (Dual Eligible)
Basically, the provider community looks to truly replace the role of the MAC and become the insurer or its own MA. It sounds simple, but it’s not. It also comes with significant risk. So how does it work and who qualifies?
How It Works
The provider becomes the insurer by becoming an MA.
- Premiums are distributed through a per–member, per-month model (PMPM) through a negotiated bid process with CMS.
- 85% of the PMPM payment must be used for care. Unused monies are subject to recoupment.
- 15% of the negotiated rate is for administration of the program.
Qualifying Criteria
- Star rating must be 3 or more. 4 or 5 stars are preferred.
- Become a MA.
- Create a model of caring in place.
- Strong leadership and medical management.
- Competent and compliant administration.
- Bid for payment.
- Execute through a separately created provider-sponsored organization.
It sounds like this might be a great concept for any provider that wants to control its own destiny. Not so fast. This process takes more than a year to develop and assumes a significant amount of risk, financial resources, and regulatory oversight. The positive side is that the I-SNP allows the provider greater control over the delivery of care and increased utilization.
As PHM continues to gain traction, be certain we will continue to provide further detailed commentary.



















